Ministry of Health: Prescribing Partnerships
By: Katlin Abrahamson & Christine Yan
The Ivey Business Review is a student publication conceived, designed and managed by Honors Business Administration students at the Ivey Business School.
The Cost of Care
Local Health Integrated Networks (LHINs) were established by Ontario’s Ministry of Health and Long-Term Care (the Ministry) through the Local Health System Integration Act of 2006, a move designed to shift the strategic management of healthcare provision into the hands of communities. The 14 LHINs in Ontario are each responsible for the planning, funding, and integration of hospitals, support services, and long-term care facilities for their respective regions. The goal of this decentralized control is to create a patient-focused system where local coordination drives effective and efficient management of healthcare, improving care and service for Ontarian patients. Though the management of operations and distribution of funds among service providers is handled entirely by each LHIN, the quantity of funding provided to each LHIN is determined by the ministry.
However, with an aging population, the opioid crisis, and increasing emergency room visits, hospital overcrowding has become a high priority threat to the LHINs’ mandate. According to a survey conducted by the Commonwealth Health Fund, 60.5 per cent of Ontarian respondents had to wait more than a month to even see a doctor about a concern. This figure remains in line with Canada’s extremely high average of 58.5 per cent, and measures well above comparable countries such as the U.S. and the U.K., with 25.3 per cent and 42.5 per cent, respectively. Additionally, the same survey showed more than 50 per cent of respondents believed Ontario’s healthcare system required “fundamental changes” to be more effective.
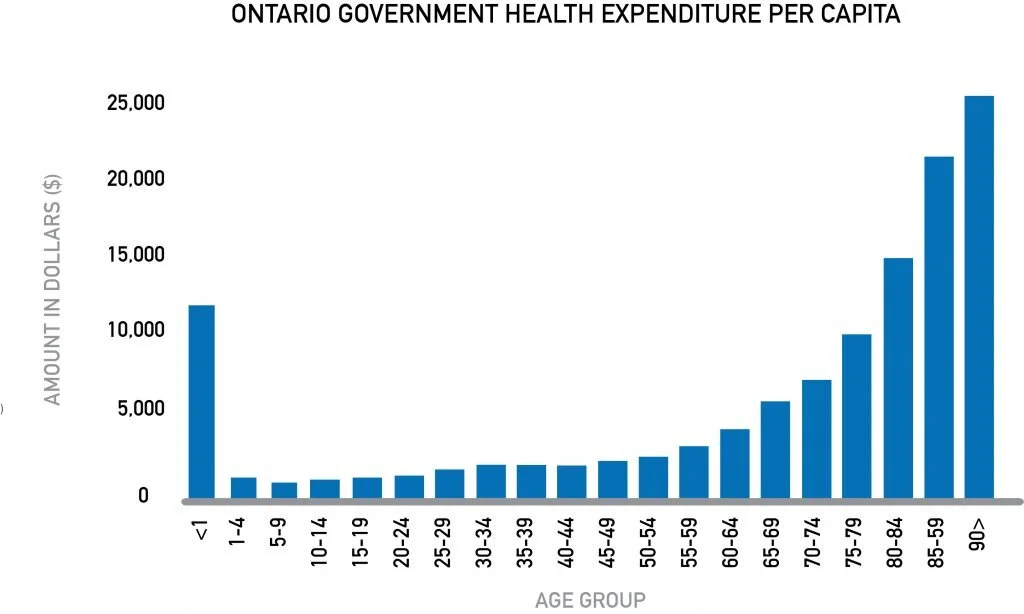
To combat the shortage of beds, the Ontario government announced in 2018 the addition of 6,000 new long-term care beds within hospitals and long-term care homes across the province, as a part of a larger plan to add 15,000 beds within five years. However, even with the province’s plan to add C$6.9 billion to healthcare spending from 2017 to 2020, it will still be difficult for the province to keep up with healthcare demand.
Technology Can Provide the Remedy
As alluded to by the Financial Accountability Office, the budget allocated to each LHIN will be insufficient for capacity requirements, as projected costs—driven by health inflation, an aging population, and population growth—are expected to outpace projected funding from 2018 to 2023. A sustainable solution to the healthcare crisis must come from innovations that can improve the LHINs’ capacity and resource management and ultimately, quality of care.
One avenue of innovation that has been underexplored by Ontario health care providers is technology, which has high potential as demonstrated by its applications abroad. For example, Baltimore’s Johns Hopkins Hospital implemented General Electric (GE) Healthcare’s Command Centre, which uses artificial intelligence (AI)-powered technology to detect real-time patient-specific delays and bottlenecks. The NASA-inspired Command Centre acts as an intersection between people and technology. In its first year of operations at Johns Hopkins, the Command Centre’s efficiency improvements in physician staffing and patient care prioritization created the equivalent of 16 new virtual beds. GE’s Command Centre has also been successfully implemented in Toronto’s Humber River Hospital, with 10 other projects in progress as of 2018.
The Biggest Barrier to Innovation
Despite widespread acknowledgement that technology can greatly improve the efficiency and capacity of hospitals, lack of funding has posed a barrier to LHINs’ adoption of this technology. The government of Ontario has made efforts to focus on market-ready technologies, setting aside C$20 million for the Ministry’s Health Technologies fund. However, depending on the size of the hospital, it can take anywhere between C$5 million and C$20 million to implement technology like the GE Healthcare Command Centre. If LHINs want to invest in technology at a scale that can lead to immediate, widespread impact, they must look towards alternative funding strategies.
Forming Public-Private Partnerships
Instead of pushing the government for more funding to invest in technology, LHINs should encourage the Ministry to enter public-private partnerships (P3s) with investors and technology companies which offer resource-management innovations like GE’s Command Centre. P3s are arrangements between government agencies and private-sector companies to finance, build, and operate projects. The increasing prominence of P3s in public services, mostly related to infrastructure in the transportation industry, is a signal of confidence in their ability to align the interests of public and private stakeholders while addressing societal needs.
The P3 solution that the ministry should adopt involves two components: first, securing the funding for investments by issuing ministry-backed bonds, and second, alleviating the service gap by implementing technology.
Issuing P3 Bonds
To address the funding shortage, LHINs interested in implementing command centre investments should, in aggregate, issue structured bonds through the Ministry. These P3 healthcare bonds would involve the provincial government as the public stakeholder and institutional investors as the private stakeholders. In addition to regular coupon payments, investors would also receive a performance-tied payback.
Many investment institutions will hold stable healthcare instruments as a means of diversifying their portfolios. Though already prevalent in current portfolios, as Canada’s senior population grows, the industry may see a larger shift towards healthcare investments. P3 LHIN bonds can play a role in these investors’ portfolios by offering stable government-backed returns. Certain institutions— particularly those with a stake in the well-being of the public—like insurance companies may be particularly inclined to purchase P3 LHIN bonds.
These bonds would allow the LHINs to establish a pool of financial capital to support their hospitals’ efforts to increase efficiency and service capacity through technological innovation. Take, for example, the Central LHIN, which oversees healthcare for the York and South Simcoe regions of Ontario. For its seven major hospitals, the Central LHIN would employ C$90 million in raised capital to finance the installation of GE Command Centres based on estimates of investment cost per hospital bed. Assuming the same increases in efficiency, cost savings, and revenue growth as at Humber River Hospital, the Central LHIN could enjoy benefits in excess of C$35 million annually.
The bonds issued to investors would consist of a three-per-cent coupon rate as well as a performance-linked payback. If 15 per cent of the cost savings are returned to bondholders through the performance-payback in addition to the coupon, investors of the Central LHIN project could expect returns of 8.8 per cent annually, with a sensitized range of approximately 6.6 to 11.5 per cent. Moreover, the interest, as well as 20-per-cent annual principal repayments, would be completely covered under the annual cost savings and increased revenues, with a net C$9 million annual bottom-line contribution over the first five years, and C$35 million in each subsequent year. Ultimately, these healthcare bonds would allow LHINs to establish a pool of capital separate from the strained Ministry budget to support their hospitals in increasing efficiency and service through technological innovation.
Implementing the Treatment Plan
The biggest risk this solution poses to the LHINs is the implementation risk of technological investments. The attractiveness of the P3 bond to both investors and the government is linked to the potential cost savings realized by the technology the bonds will fund. For the LHINs themselves, the improvements to resource management and thereby, quality of care, can only materialize through careful management of the implementation process and evaluation of the associated impact.
Because the pool of bonds would be issued and backed by the Ministry of Health, oversight and distribution of the funds generated from bond issuance would still fall to the ministry. Each year, LHINs would apply to add new projects to the pool, with details about each hospital’s project, the expected increase in capacity, and cost savings. This should be done to ensure that individual hospitals in LHINs can tailor the project to their specific needs while implementing a system of control that delivers assurance that the LHINs as a whole will achieve performance goals.
Once the hospital has obtained the necessary funds, due to the complexities of the healthcare system, the LHIN’s greatest focus should be placed on stakeholder buyin. At Humber River Hospital, implementation of the GE Command Centre resulted in front-line workers’ opposition due to an initial fear of losing decision-making power. To achieve the support of staff, the hospital engaged them during the entire planning and implementation process including the curation of efficiency metrics, technology integration, and testing. This allowed the hospital to experience the benefit of increased efficiencies and improved patient prioritization.
The final step of the implementation process would be for the Ministry to evaluate the different innovations at the hospitals to which they provide funding. To do this, hospitals will need to track and report the cost savings and operational efficiencies realized through the implementation of the technology. An impact assessment based on these metrics should be required for hospitals to understand the comprehensive effect of the technology on hospital capacity and quality of care. If hospitals have implemented technologies like GE’s Command Centre, the highly-sophisticated nature of AI-powered, datadriven technology will be able to self-monitor and report, eliminating the need for additional hospital resources to measure the results. Such an impact assessment would not only provide investors with transparency during the process of allocating annual savings bonuses but would also help LHINs establish a benchmark against which future applications for funding could be evaluated.
Public and Private Prosperity
An aging population with increasingly complex needs and public spending constraints are leading to an inevitable healthcare crisis for the Canadian population. The two-fold P3 solution would allow the LHINs to better satisfy their commitment to the population they serve by increasing capacity. Issuing healthcare bonds to invest in technology would not only expand hospitals’ capacities, but would provide a sustainable approach to healthcare’s financial woes. Ultimately, greater hospital efficiencies would allow the LHINs to improve quality of care as frontline healthcare workers spend more face-to-face time interacting and providing a personal touch to patients. Reaching to the private sector and forming P3s to invest in efficiency-enhancing technologies in hospitals is imperative to retain the integrity of the public healthcare system